Busting Top Trauma MythsBY KEVIN T. COLLOPY, BA, FP-C, CCEMT-P, NREMT-P, WEMT, SEAN M. KIVLEHAN, MD, MPH, NREMT-P,SCOTT R. SNYDER, BS, NREMT-P ON MAR 2, 2015
The myth explained
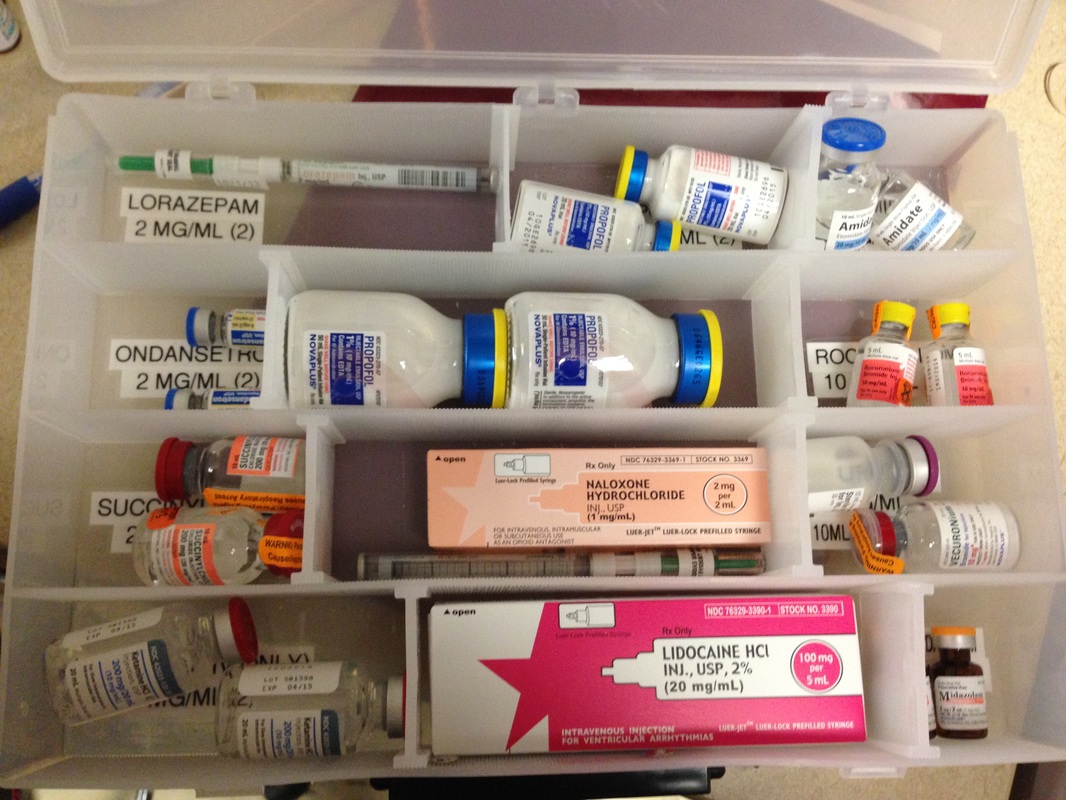
It is known that laryngeal manipulation and endotracheal intubation are both associated with a transient rise in intracranial pressure (ICP), and patients who have a head injury with increased ICP are considered at an increased risk for secondary brain injury. Since a transient ICP rise could decrease cerebral perfusion pressures, every effort is made to control ICP. In theory, lidocaine prevents this transient ICP rise, which helps prevent a secondary brain injury. Evidence for lidocaine as a preventive measure first appeared in 1980, when Robert Bedford, et al., published their paper, “Lidocaine prevents increased ICP after endotracheal intubation,” when they monitored 20 patients who were undergoing elective neurosurgery. Their results showed that while patients who received lidocaine did experience a rise in ICP, it was significantly less than in patients who received a placebo. Ultimately, these results were extrapolated to use lidocaine as part of the medication sequence for intubation, although this study did not address this question at all.
The Evidence
Drs. Mike Clancy and Neil Robinson reviewed all of the available literature regarding the use of lidocaine in RSI and published their findings in 2001. After an exhaustive literature review, they only found six papers that addressed lidocaine and intracranial pressure changes. No paper studied lidocaine during RSI. These authors concluded there is no evidence to support the use of lidocaine as a clinical intervention during RSI and recommended its administration be limited to clinical trials.
Although there is no evidence to support the use of lidocaine, is there evidence that suggests that lidocaine causes harm? A 2012 paper in the American Journal of Emergency Medicine determined lidocaine had no impact on the hemodynamic stability of patients receiving RSI following traumatic injury and determined the drug was safe to administer during RSI.
However, one potential problem is that lidocaine administration is time-dependent. Some authors suggest that to have any potential benefit for the patient receiving RSI, lidocaine must be administered at least 2 minutes prior to laryngoscopy. Waiting an additional 2 minutes to intubate a patient with a head injury may be its greatest risk, as during this time patients can remain hypoxic, potentially aspirate and continue to fight, which further exacerbates an increased ICP. Lidocaine has a dose-dependent effect as well and too much lidocaine can be detrimental. While minimal arterial blood pressure changes occur when patients received 1.5 mg/kg of lidocaine prior to neurosurgery, significant blood pressure declines occur when the dose is increased to 2 mg/kg.
The Bottom Line
Lidocaine is not proven to prevent a rise in ICP during RSI. While it may not directly harm patients, its administration does delay the completion of RSI, which puts the patient at risk for continued hypoxia.
Read More...
http://www.emsworld.com/article/12043670/prehospital-trauma-myths